Preeclampsia is a term that seems to get thrown around pretty casually when moms-to-be talk about pregnancy complications. In reality, it can be life-threatening. Get the lowdown right here, from causes to preeclampsia diets.
Often arriving without symptoms, preeclampsia is a potentially serious complication of pregnancy that can cause problems well into the rest of your life. Overwhelmed by all the information that’s already out there? Find out everything you need to know.
What is preeclampsia?
Preeclampsia in pregnancy is a condition that is believed to be associated with the placenta not working properly, although preeclampsia causes are not fully understood. It usually affects women in the later stages of pregnancy, from around 20 weeks onwards. It’s relatively common, with some estimates suggesting that preeclampsia affects between 2% and 8% of worldwide pregnancies.
Although most outcomes are good, preeclampsia isn’t something to take lightly, with around 10% to 15% of maternal deaths associated with the condition. If preeclampsia isn’t treated in time, it can cause complications, including blood clotting disorders, stroke, organ problems, eclampsia—which causes grand mal seizures—or HELLP, a syndrome in which women are at risk of bleeding to death. One of our writers experience HELLP syndrome with her first baby—here’s what she learned from the experience.
And preeclampsia isn’t just physical, according to Shoshana S. Bennett, PhD, co-author of Beyond the Blues: Understanding and Treating Prenatal and Postpartum Depression & Anxiety. Dr. Bennett says, “Depression during pregnancy and postpartum (PPD) is increased significantly when health complications arise. As perinatal psychologists, we frequently encounter women whose depression and anxiety directly relate to their experience with preeclampsia.”
That all sounds fairly heavy, but if you do develop preeclampsia, remember that it is common in women who are close to giving birth.
Preeclampsia symptoms
Preeclampsia in pregnancy has two main symptoms:
- Protein in your urine
- High blood pressure (hypertension)
Because the main preeclampsia symptoms are relatively difficult to spot on your own, it’s often not detected until you have an antenatal exam. Other preeclampsia symptoms may include severe headaches, temporary loss of vision, upper abdominal pain (just below the ribs), shortness of breath, nausea or vomiting, and swelling of the feet, ankles, hands, and face. Noticed any of these preeclampsia symptoms? If so, it’s important to seek immediate medical attention.
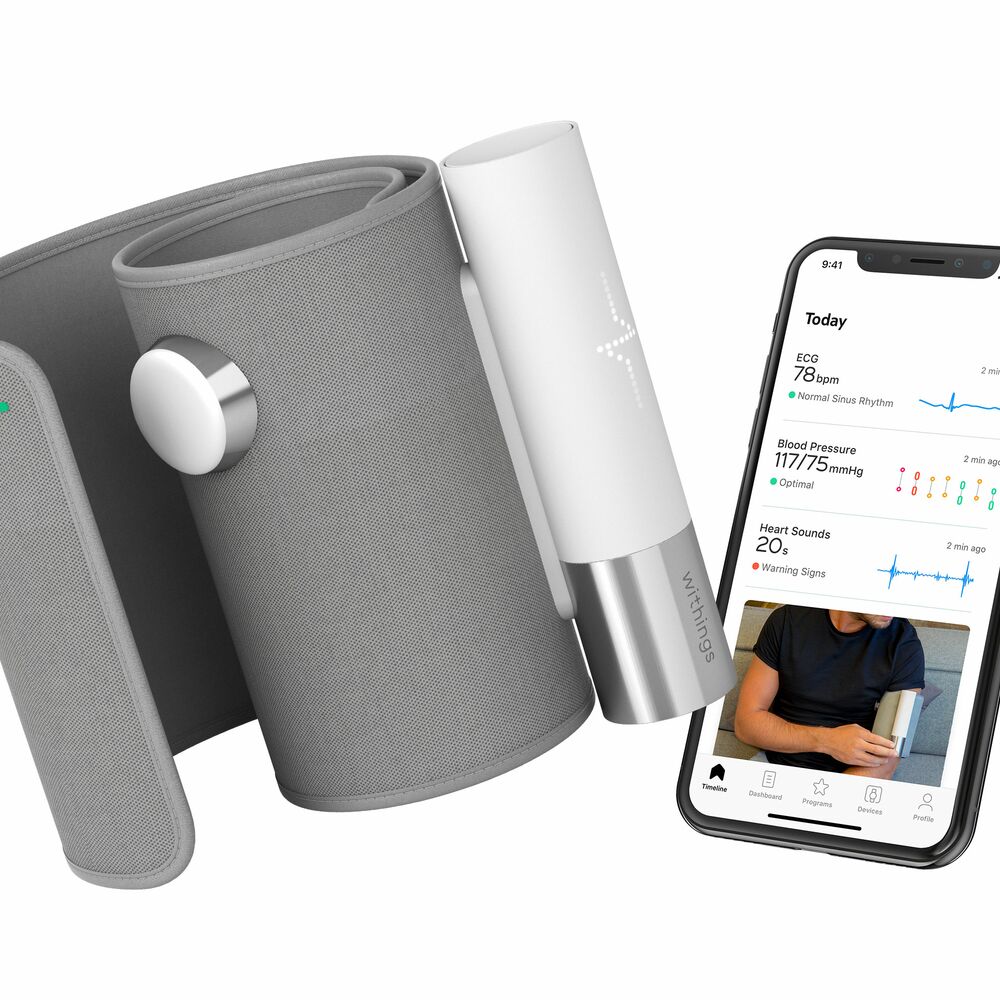
And if you want to check your own blood pressure at home, take a look at BPM, our own wireless blood pressure monitor, which allows you to check it easily and share the results with your doctor.
Preeclampsia causes
First off, it’s important to note that doctors aren’t completely sure about what causes preeclampsia. Several potential preeclampsia causes have been identified, including diet, generic factors, and autoimmune disorders. However, researchers are pretty sure that it has some sort of connection to the placenta. In the early stages of your pregnancy, new blood vessels will develop so that your body can send blood to your placenta—the structure that provides nutrients and oxygen to the fetus—more effectively. For women who have preeclampsia, these new blood vessels will not develop properly and nutrients that are essential for development may be blocked from reaching the fetus.
Preeclampsia risk factors
Although anyone could potentially develop preeclampsia in pregnancy, there are certain factors that can increase your risk:
- Having high blood pressure
- Having Type 1 or Type 2 diabetes
- Having an autoimmune condition like lupus
- Having a chronic kidney disease
If you fall under any of these categories, you should take the time to schedule an appointment with your doctor or midwife. There are several other things that can slightly increase your chances of developing preeclampsia, including a family history of the condition, a 10-year gap (or more) between pregnancies, a BMI of 35+, expecting multiple babies, and being over 40 years old.
Preeclampsia treatment
It’s difficult to prevent preeclampsia in pregnancy, partially because doctors don’t wholly understand the mechanism behind it. If your doctor suspects that you do have preeclampsia, there are several diagnostic tests that they may run, including urinalysis, blood tests, or a fetal ultrasound. Treatment is usually handled on a person-by-person basis. In general, the aim will be to deliver the baby as quickly as possible, preferably before any major complications can occur. In lieu of induced labor, your doctor may also recommend bed rest, medication to lower blood pressure, and for you to drink lots of water.
It may be possible to reduce the risk of preeclampsia with a preeclampsia diet. According to Babycenter.com, a calcium-rich preeclampsia diet consisting of foods like cheese, milk, yogurt, and kale may reduce your risk, while foods with plenty of vitamin D are also recommended. Taking supplemental vitamin D may also be worthwhile.
For a really long time, people believed that the cure for preeclampsia was birth. Once the baby popped out, everything went back to normal. Now, this isn’t exactly true. In fact, 97% of preeclampsia deaths happen in the postpartum period. That’s not to say that post-birth preeclampsia complications are anything like the norm. In most cases, preeclampsia will improve soon after the birth of your baby, but it’s just important to remember that at any point in the first six weeks after you give birth, there’s a risk of postpartum preeclampsia.
Be on the lookout for preeclampsia symptoms like stomach pain, severe headaches, nausea, or swelling, and if you do notice anything, call your midwife, doctor, or OB/GYN immediately and head to the emergency room.
We hope this post has given all the moms-to-be out there some extra insight into the surprisingly scary condition of preeclampsia. The bottom line is that even though it’s certainly something to take seriously, you may be able to keep yourself and your baby safe through timely medical treatment.